Parenting a PDAer with Non-24
- Dara Hutchinson
- Apr 23, 2023
- 18 min read
Updated: Jun 27, 2024
Up to 80% of autistic children have a sleep disorder, and E happens to have a rare sleep condition that has added another highly complex layer to our family's experience. At the height of his burnout crisis at age 6.5, E's sleep times became out of synch with the world's day-night cycle and he developed a circadian rhythm disorder called Non-24 Sleep-Wake Syndrome.

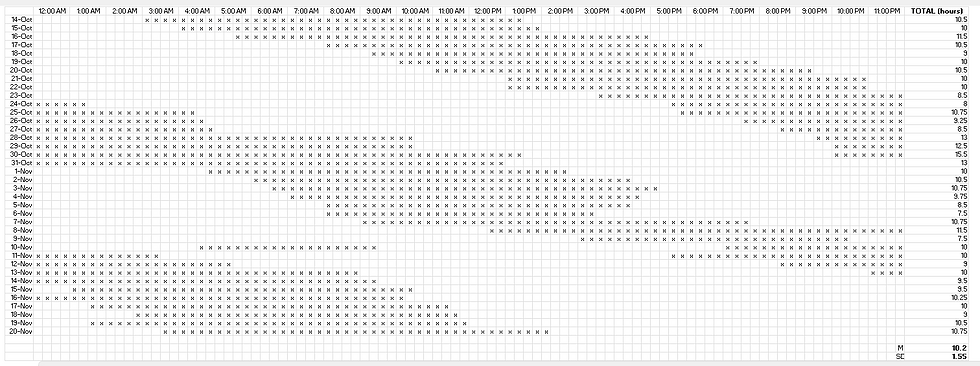
Most people sleep and wake at roughly the same time each day because the suprachiasmastic nucleus (SCN), the brain's master clock, synchronizes daily to the light-dark cycle of the earth. For individuals with Non-24, however, the SCN is desynchronized from the world's light-dark cycle and cannot reset daily, thus running longer than the typical 24 hours (or in a few extremely rare cases, shorter). As a result, individuals with Non-24 do not sleep and wake at the same time each day. Instead, their sleep and wake times progress forward an hour or two every day and cycle continuously around the clock. The graph below is a sample of E's sleep log from Fall 2022. The forward progression and cycling nature of his natural circadian rhythm is a classic example of the pattern of Non-24 Sleep Wake Syndrome.
Non-24 is most prevalent in the totally blind when it is caused by light not reaching the SCN to reset the body's clock on a daily basis. For many professionals, this is the only iteration of Non-24 they are familiar with. However, the condition can also occur in sighted populations, occasionally due to a brain injury, or, as in E's case, co-occurring with autism. More research is needed about the link between Sighted Non-24 and autism, but in autistic people, it is thought to be caused by differences in the production of melatonin, and environmental factors may also play a role.
Like PDA, Sighted Non-24 is not well known or understood by professionals. Because many people with Sighted Non-24 must force their bodies to sleep and wake at typical times to be a part of society (go to school, hold a job, attend appointments, etc.), they can't cycle around the clock on their natural schedule and probably don't know that they have a natural Non-24 pattern. They may seek help initially because they suffer from unusual periods of insomnia and excessive daytime fatigue when their circadian rhythm is in the nocturnal part of their cycle, then they may feel well for a few days when their circadian rhythm lines up with the earth's day-night cycle. Over time, individuals with Non-24 who must keep to a typical schedule will suffer from sleep deprivation and its many serious side effects.
Alternatively, some people with with Non-24 may find out they have the pattern if their lifestyle allows them to "free run," which is the term for letting the body sleep and wake according to its own natural rhythm. We discovered E had a Non-24 pattern when we let him listen to his body about when to go to sleep.
When E was at the height of his burnout crisis at age 6.5, we were just discovering PDA and beginning to make the recommended accommodations to stabilize his nervous system. As I have explained in previous posts, E has an intense fight response so increasing the safety of our home and decreasing his aggression was our number one priority at that point in time.
Because bedtime had always been one of the most challenging parts of our day (often a two or three hour physical fight that was traumatizing for everyone and only ended when E eventually collapsed from exhaustion), we decided to pivot from the traditional parenting approach to bedtime and instead allow E to listen to his body about when he was ready to sleep. We assumed he would settle into a later bedtime and wake later in the morning, which would have been fine because our homeschooling schedule gives us plenty of flexibility. Of course we had never heard of Non-24, nor imagined his sleep would ever become as dysregulated as it did. We were in for a surprise!
After we relaxed our bedtime expectations, the fight-or-flight behaviour surrounding sleep disappeared. The aggression stopped. Yes, he started staying up later, but we anticipated that and were ok with it initially. Everything seemed to be working out. E would go to bed around the same time as us with no fuss. After a few weeks, however, he was keeping himself awake even after we went to bed (the novelty of being up late was at this point was enough to keep him content about being awake alone, but that would soon fade). We knew he was up much later than most 6-year-old's, but he was happy and not aggressive and still getting enough sleep so it was fine.
Then, one more morning when I went to get the baby when she woke at dawn, I found E still awake in his room playing Minecraft!! I was shocked and I remember admonishing him, "What are you doing still awake?!?" He said he just couldn't sleep so he decided to play some more Minecraft. That was the first time he stayed awake all night. He slept that morning, then stayed up even later the next night, slept in again, then stayed awake later, and so on. Within a week of that initial all-nighter, his sleep had shifted into a cycling pattern. I started tracking the times because I could tell it was so unusual; he wasn't just staying up late, he was cycling around the clock. I had never heard of anything like this. A few weeks later, I learned of Non-24 through a PDA support group and, like our initial realization about E being autistic, it was another light bulb moment. Our child fit the criteria for not one but two little-known conditions.
In those early days of living with Non-24, we attempted to get his system back on track with typical sleep hygiene suggestions like waking him at a certain time each day, monitoring or even restricting screen use after dark, keeping evening lights dim, encouraging morning sunlight, etc., but all of these typical suggestions activated his threat response to unsafe levels because E perceived the demands of sleep hygiene as a threat to his autonomy. He was still in such a precarious state of near-constant fight-or-flight that any comment about sleep or bedtime would push him over the edge and he would become aggressive. So, we decided to put safety first and let him sleep when his body needed to. Radically accepting his sleep pattern in this way, while also lowering demands in other areas of life such as meals, screens, and personal care, allowed E's nervous system to rest. We saw a reduction in fight-or-flight behaviour almost immediately. Lowering demands worked to help him heal.
However, E can't be awake alone and my nervous system is his primary source of regulation, so he required my presence most of his waking hours, day or night. If I tried to hold firm boundaries about my own needs around sleep, insisting that I could not get out of bed to play with him in the middle of the night, for example, he would become unsafe. Declaring myself unavailable in the nighttime hours triggered his threat response. So, I made the decision to accommodate instead of escalate his nervous system and I would get up when he needed me, no matter what the time of day or night. Like his nervous system disability, E's sleep pattern is not his fault. Non-24 is a neurological disorder. He cannot control how melatonin is released in his body any more than he can stop his overwhelmed system from going into fight-or-flight.
That is the true crux of our sleep situation; I was left with the terribly difficult decision of having to choose between meeting E's needs for sleep and well being, or meeting my own. At that point in time there was no feasible way to do both. So, he slept on a Non-24 schedule, and I slept when I could. My husband and I knew this was not a sustainable solution, but it was all we could do at the time.
I was learning more about Low Demand Parenting at this point and becoming very aware that although we were lowering demands for E and seeing the benefits to his nervous system, the demands on ME were extremely high. Ideally, with the low demand lifestyle, families find a way to meet everyone's needs without anyone having to work beyond their capacity, adults included. In traditional parenting, we expect the child to rise to the parent's expectations; in Low Demand Parenting, we drop the demands that are too hard for our children and instead come alongside them to radically accept where they are at. That's what I did with E's sleep. Then, the crucial part of making this lifestyle sustainable for everyone, is that the parents work creatively to meet their own needs without asking anything different of their child. I cannot control when E sleeps. So, I radically accept that this is a terribly difficult season in our life. I accept all the anger, grief, frustration that arises in me. I acknowledge all the feelings, and let them go. Non-24 is no one's fault. Then I move on to finding proactive ways to lower demands for myself so I can support my own nervous system through this difficult time, so I can survive with some semblance of sanity, and continue to support E in the process.
As I wrote in earlier posts, we made drastic changes to our family structure in the fall of 2021 when E was at the height of burnout; for example, we hired caregiving support and enrolled B in a part-time preschool program. These two major changes helped immensely with not only the safety of our home, because the children could be separated, but they also helped our sleep situation because, if E was in a nocturnal period, I was able to nap when our caregiver was here or sleep while B was at preschool.
Although I had always been E's preferred parent, I soon realized that I could not be the only one responsible for being awake overnight, no matter what E might want. So, I had to be very clear about my needs with my husband and ask him directly for help. He is a wonderfully creative problem solver and came up with this solution; he installed Minecraft on one of the powerful computers in his lab, one that can run the more graphics-heavy RTX maps that our computer at home could not, and he started taking E to work with him in the late evenings when E was nocturnal. My husband has always been a night owl and through the journey with our son he has realized that he, too, identifies as autistic, and he has sleep differences of his own; his innate "night owl" tendencies are indicative of a circadian rhythm disorder called Delayed Sleep Phase Syndrome (DSPS). Since he naturally prefers to be awake later at night and sleep later in the morning, my husband moved all his work commitments to the afternoons and began staying awake with E in the late nights and they would go to his lab in the middle of the night. My husband would work and E would play Minecraft on the fancy computer, and they were both happy. The fact that his job allows him such flexibility, and that his boss was understanding of our situation, was immensely helpful in seeing E through the nocturnal weeks. I would go to bed not long after B did (she had a typical toddler bedtime of about 8 pm) and sleep as long as I could. My husband would stay awake with E until 2 or 3 am, then we would switch shifts and he would sleep until about 10 or 11 am before going into work for the afternoon and evening hours and coming home for a late dinner by about 7. So, when E was completely nocturnal, I was still only sleeping 5-6 or so hours overnight, but combined with the lowered demands elsewhere, it was enough to survive through burnout, just.
I lowered demands for myself in many ways during this period in order to support my own nervous system. I thought about the times of day that were the hardest for me and then thought specifically about what it was that was hard in that moment, what need of my own was not being met, what I could do for myself to meet that need, and what choices I could make in those hard moments that would support my own nervous system. Intentionally naming and meeting parental needs in this very small and specific way is part of Amanda Diekman's Low Demand Parenting Approach. No, it is not enough - what I really needed was to sleep all night, every night, but at least it was something. Ideally, I would love to have full-time, live-in caregiving support from someone who my children would happily accept in my stead so I could have ample time to rest and heal and take care of myself in both big and small ways. But that is a fantasy. In reality, my child has a nervous system disability, my family has financial constraints, we were helping each other and ourselves in every way we could think of, but it was still not enough. So, l dropped every demand on myself that I could throughout the day, and chose wisely how I spent my glimmers of free time. Those were the things I could control. The teeny tiny moments of self care throughout the hardest parts of the day added up to be enough for me to survive the sleep deprivation.
For example, I started having groceries delivered to lower the demand of even having to leave the house to do a pick up of my online order (not being able to leave if E was asleep in the day was something I had to learn to work around in many situations). I subscribed to Hello Fresh for easy, tasty, nourishing dinners for me and my husband without having to think about meal planning (the kids ate some parts of the meals sometimes, and other times I made them their safe foods instead and that was fine). I kept the fridge and freezer stocked with convenience foods I liked, like Amy's frozen meals, so I could feel satisfied by yummy food even if I didn't want to cook at all.
I bought more of the clothing that met my sensory needs for soft, comfortable fabrics day and night (I made myself a uniform of sorts buying multiple of these t-shirts, these leggings, and these cozy sweaters). I was always comfy, plus on the occasions that E would still go into fight-or-flight and bite holes in my clothes, I wasn't too frustrated because they were affordable and accessible enough to easily replace.
In addition, I found I was often too tired to get ready for bed and the sensory experience of the bathroom, the lights, the water, felt overwhelming to my frazzled nerves, but I also hated the feeling of going to bed without cleaning away the day. So, I got into the habit of brushing my teeth when getting B ready for bed so that was one bedtime task of my own done early, and I got compostable facewash wipes and kept them in my bedside drawer, along with my hairbrush, lip balm, and lotion, and this small switch of having these items beside my bed and not needing to go to the sink to get ready was small but very supportive. I could still feel "ready" for bed, but not have to walk the extra 20 feet to the bathroom sink because that simply felt like too much of a demand.
I also became more comfortable with our caregiver helping with household tasks like dishes, laundry, or taking out the garbage. On days when I knew I would have help, I dropped the demand for myself to do these things before she came over. I was also clear with my husband about not being able to participate in house renovation projects; if he wanted to continue working away at things, that was wonderful, because our house really needed it, but I needed to conserve my energy and did not want to sand baseboards, thank you very much. Similarly, when he came home from work, I almost immediately excused myself to go lie down. He was slightly hurt because he wanted to chat and share about the day, but I knew I was depleted and didn't have the capacity to have an adult conversation without becoming irritated and overwhelmed.
In general, I stopped feeling guilty about not being able to do it all. I protected my energy. I didn't mop my floors for months. I didn't touch the dishes for 3 days and ate cereal for dinner out of a measuring cup. And I was actually ok with this. I became comfortable with doing just enough. I had to. I made time for things that filled my soul, like playing my guitar, learning the piano, reading historical fiction with strong female protagonists, doing a crafty project like embroidery, working outside in our yard, or just crawling back into bed under the thick duvet with a pillow over my head and curling up in the fetal position for 10 minutes because that felt good. I had such little time for myself, the time I did have had to be spent doing things that were restful and that brought me joy.
For a year and half, I survived in this knowingly sleep deprived state, supporting my nervous system as best I could, because it is what was needed to get E out of burnout. I truly believe that giving him the freedom to sleep according to his own body's signals was an integral part of his recovery. For a child with a nervous system disability who needs autonomy to feel safe, having the ability to sleep when he was tired and wake when he was rested was the highest form of freedom we could give. Throughout his recovery, although he was sleeping at atypical times, he was getting plenty of sleep. We know from tracking his sleep that his daily average was 10.4 hours, well within with the recommended range for his age. Getting the sleep he needed, when he needed it helped him heal. I'm sure of it. So, it was worth it in that regard. And it was exceedingly difficult for me to sacrifice my own sleep. Both of these things can be true.
Over the last year and a half, E's sleep has affected our family as much if not more than his sensitive threat response; while the intense aggression has faded, the Non-24 sleep pattern persists. As Casey Ehrlich of At Peace Parents has noted, while most PDAers experience difficulty with all basic needs during burnout, one need tends to be the "stickiest;" the one they struggle the most with is usually the need that was also an issue pre-burnout (E was never a "good" sleeper and bedtime was challenging for years), and continues to present challenges post-burnout. For E, his "stickiest" basic need is most definitely sleep.
In the last few months, we have been able to make progress in getting his sleep to align better with the needs of the rest of the family. Since E is now out of burnout and growing ever more steady on medication, his nervous system can handle the difficult problem solving conversations about parental needs. Because he is out of burnout, he has a responsibility to now contribute to the well-being of the family as a whole and help me and his father get the sleep we need, just as we helped him when he needed it most. Putting that responsibility on an 8-year-old may seem like a lot of pressure, but he craves balance with those around him, so treating him as an equal member of the family, a member who has responsibilities as well as needs, is the phase we must move into for our family as a whole to recover. He showed great maturity in agreeing to try Risperdal again, and it just so happened that right around the time he started taking his meds regularly, we also had our long-awaited appointment with the one pediatric sleep specialist in our city.
The appointment overall was only mildly more helpful than Google, but hearing the doctor recommend melatonin and light therapy, two things I had been offering to E for years, seemed to be help in the sense that hearing them from someone outside the family was beneficial. He agreed to try melatonin and light therapy to see if his circadian rhythm could be reset.
Interestingly, the doctor did caution that, in his understanding, Non-24 is a very specific neurological condition that he could not say for sure E did or did not have. Although we have indisputable data from tracking E's sleep that clearly points to a Non-24 pattern, there is no easy way to test whether or not his circadian rhythm is out of synch because of underlying neurological differences, which would be Non-24, or because of environmental reasons, which, according to this doctor, would not officially be diagnosable as Non-24. When blind individuals experience Non-24, the reason is clear; light cannot physically get to the SCN. In Sighted Non-24, however, it's harder and more nuanced to officially diagnose the condition because the causes are less understood.
Is it possible that environmental factors during burnout, such as spending long hours a day on a screen inside a dark room where he could not tolerate the blinds being open, let alone tolerate spending time outdoors, contributed to the development of Non-24? Yes, of course. Is it also possible that he already had underlying neurological differences in the production of melatonin that made him more susceptible to circadian rhythm differences? Yes, of course.
As with most things in life, it is likely a mixture of nature and nurture. None of the professionals we have worked with, even the pediatric sleep specialist, have any experience working with an autistic child with Non-24. None of them have prior knowledge of PDA. The combination of these two little known conditions makes it very challenging to get the right support from the traditional medical, educational, and parenting establishments. Typical rules do not apply to our situation. We are out here doing our best with very few others to pave the way for us.
Through my research, I have made contact with a handful of families around the world who also have a PDAer with Non-24. All of them are allowing their child to free run and doing what they can to support the rest of their family along the way, just like we are. I've learned autistic adults with Non-24 that, in general, having to adopt a typical schedule for work or school is not ideal. Adults with Non-24 have a better quality of life when they can free run. This is possible with the help of free lance work, disability benefits, supportive work and school environments, and the understanding of family and friends. If E were a few years older and content to be awake alone during his nocturnal periods, I honestly would have no problem with him continuing to free run; he healed from burnout and taught himself to read and write all while sleeping on an atypical schedule. He is thriving. And I am breaking down from sleep deprivation. My mental and physical health has declined. If I continue to be sleep deprived, I worry about eventually having to go away for a while and check myself into a hospital to recover. The burden my absence would cause our family would be immense. So, we need to figure this out!
For a few months after seeing the sleep specialist in February, E took the melatonin before bed and we gave powerful light therapy an hour before his usual wake time. These supports, along with the Risperdal, a second generation anti-psychotic that works as a mood stabilizer, but also stabilizes all the body systems, including sleep, were enough to hold his cycling sleep steady with a delayed sleep phase. This was a huge breakthrough! I could go to bed at a normal time, E and my husband could stay awake until 2ish and then they would both sleep until midday. This rhythm actually worked well for our family.
But, it was too good to be true. The melatonin proved to be too much of a demand for E and he stopped taking it (instead throwing the gummies at me or my husband when we brought the dose to him). Declarative language didn't help, choice about flavour or treats alongside the gummies didn't help, exploring different forms of melatonin like chewable or tablets didn't help. His sleep started slowly progressing forward again, from 2 am, to 3 am, 4, 5, 6, 7. After about 3 am, my husband can no longer stay awake, so I went back to doing my early bedtime after dinner and then getting up to switch shifts in the early hours of the morning.
A few things have changed though, since the last time E was free running. He is slightly older and his nervous system has stabilized enough that he can tolerate watching shows or playing video games by himself for a few hours so I can nap. So, if he is nocturnal, I will switch shifts with my husband around 3 am, spend time with E for a few hours, fix him a snack, and then be able to sleep a few more hours before our daughter wakes around 8. E would not have been able to handle this during burnout. That is progress.
Another change, though not a positive one, is that the physical and mental health symptoms of sleep deprivation that took months to appear for me when E first started free running, (because, I assume, my body was previously healthy and I had enough reserves to deal with short term sleep deprivation) now reappear after even one night of not enough sleep. My hands shake. My head hurts. My body aches. I feel nauseous. I'm irritable and my patience is thin. My anxiety and depression spike. I feel hopeless. My symptoms of PTSD worsen. My auditory hallucinations return. Obviously, this is my body crying out saying, "We can't handle any more of this! You need sleep or we are going to completely break down!!" I know this. I hear you, body! AND, E still can't regularly be relied upon to sleep all night, and still can't be awake alone.
So we are brainstorming more creative solutions.
Perhaps a caregiver who would be willing to work night shifts (and whom E could tolerate in my stead)? Possibly, but it has taken upwards of six months for him to be comfortable enough with other caregivers to stay alone with them, so it's uncertain whether he could handle someone else's coregulatory presence at night while my husband and I sleep.
Perhaps other forms of melatonin? I just bought liquid drops and his favourite pop to try.
Perhaps the sleep specialist will have more suggestions at our follow up appointment? Perhaps we will decide to travel to see a different specialist?
Perhaps E will continue to feel more and more comfortable alone and need us less at night and he will just keep free running?
Perhaps he will decide on his own he would like to be awake in the day to be able to do things he enjoys and he will try the melatonin and light therapy suggestions again one day?
For now, my husband works in academia and we are coming up on the summer semester, so that means he has a lot more flexibility with his schedule. He plans to follow E's sleep pattern as much as he can, because he is happy to work and sleep at odd hours, and I will will be on a typical schedule with the 3-year-old, because my body needs to sleep at night. Then after summer we will reassess again.
Honestly, I don't know what will happen next. But I know we have come so far, so we will get through this somehow.
Sighted Non-24 is so unknown, I've compiled a list of the resources I have found the most helpful.
These websites describe the condition:
This is a dedicated facebook group for Sighted Non-24 and autism:
This is the bigger general Non-24 group:
This is a book by adult PDA blogger Sally Cat who has personal experience with circadian rhythm disorders and has compiled her experiences and the experiences of other individuals into this volume.
These are the results of a sleep survey conducted by the PDA society:
Suzanne Gunn is a Family Sleep Specialist who is ND herself and has a PDAer of her own. She is creating a course on PDA and sleep that you can join the waitlist for. I have shared my story with her as a recording that will be part of the course module on Non-24:



Thank you SO much for sharing about this! I think this sleep issue may describe my son. I’m going to do more research. I really appreciate your gentle and positive approach to accommodations for your son. Bravo!